when a repair of the rotator cuff is decided several operative times will follow one another:
This exploration makes it possible to confirm the lesions found in imaging examinations (in particular MRI may very well underestimate tendon lesions), namely lesion of the deep or transfixing face of the tendon.
We will also look for the presence of osteoarthritis (cartilage wear), the presence of which can explain part of the pre-operative pain but also residual pain after an intervention on the tendons.
The long biceps also frequent source of pain will be evaluated.
The exploration will also include the sub-acromial space, often seat of intense inflammation (bursitis), looking for lesions on the superficial aspect of the tendons, the aggressive nature of the acromion and the inferior surface of the acromioclavicular joint.
In the first place a cleaning of the sub-acromial bursa is necessary in order to relieve by removing this very thick, inflammatory and painful tissue (in sick patients of the shoulder) but also to see the superior face of the tendons.
Acromioplasty is most often done to make the bone ceiling non-aggressive, most often resection of the coracoacromial ligament (which prolongs the acromion forward and contributes significantly to the tendon conflict).
For some surgeons of which we are a part, a gesture will be almost always performed on the long biceps, it will either be severed simply (tenotomy of the biceps) or more reinserted on the humerus in or under the bone (tenodesis of the biceps).
Finally, the acromioclavicular joint can be the place of intense inflammation also, often in the context of an early osteoarthritis at the origin of aggressive parrot beaks in contact with the tendons of the cap. It is thus the object of a planing inferior to the minimum (co-planning) to see a radical treatment by resection of the last centimeter of clavicle (suppression of the articulated patient).
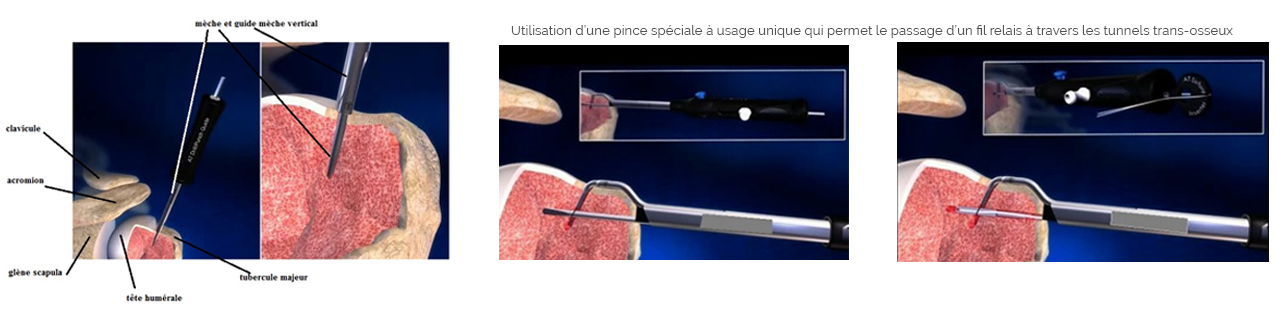
Avascularity of bone tuberosities, place of insertion of the tendons, and resettlement at these tuberosities of the tendons by means of resorbable or metallic anchors see tunnels transosseous son who will be passed through the tendons by means of pliers or needles.
The material used is only to force the tendons to heal on the bone, it does not have sufficient strength to maintain the tendon in place when using the arm. The tendons are in principle securely re-anchored after 6 weeks (allowing to operate even the arm without the risk of tearing them).
The arthroscopic exploration allows an almost complete vision of the joint, a complete assessment of the tendon lesions.
It allows to repair all types of tendon rupture.
The approach of the tendons is minimally invasive and does not require muscular disinsertion, reducing the immediate consequences and sometimes the type of immobilization.
Its difficulty, the learning curve is one of the most important and long of orthopedic surgery.
This is mainly why some surgeons who do not practice shoulder surgery regularly operate in the open. Others have become accustomed to operating by opening classically and consider having better results as well.
The goal of repairing both the arthroscopic and open-top cuff (or better) is very hard to achieve!
The cost is important, it is necessary to invest in an arthroscopy column, in special instruments and in consumable material (single use) more expensive.
However, for the surgeon who is well versed in arthroscopy, it becomes the best way to understand the shoulder and its pathologies and therefore to treat each case better.
Shoulder exploration
during an arthroscopic repair of the rotator cuff the first step is the exploration of the glenohumeral joint, in order to:
- to confirm the lesions found in imaging examinations (notably MRI may very well underestimate tendon lesions), namely lesion of the deep or transfixing tendon face.
- look for the presence of osteoarthritis (cartilage wear) which may explain some pre-operative pain or residual pain after surgery on the tendons.
- evaluate the long biceps also common source of pain.
The exploration will also include the analysis of the sub-acromial space:
- often seat of intense inflammation (bursitis),
- looking for lesions on the superficial side of the tendons,
- the aggressive nature of the acromion and frequently the underside of the acromioclavicular joint.
Bursectomy:
ablation of the most often inflammatory sub-acromial bursal tissues, this makes it possible to clean the superficial face of the muscles and tendons of the rotator cuff.
acromioplasty
Padding of the lower end of the acromion usually performed before the tendon repair (see after according to surgeon because can cause bleeding) to leave room for tendons repaired, to avoid that they conflict with its previous edge or lateral (see page under acromial conflict) and compromises their healing.
In cases of acromioclavicular lower osteophytes the resection procedure will be prolonged at this level (almost systematic for us) because the reasoning is the same as for the acromion concerning the wear of the tendons of the cap
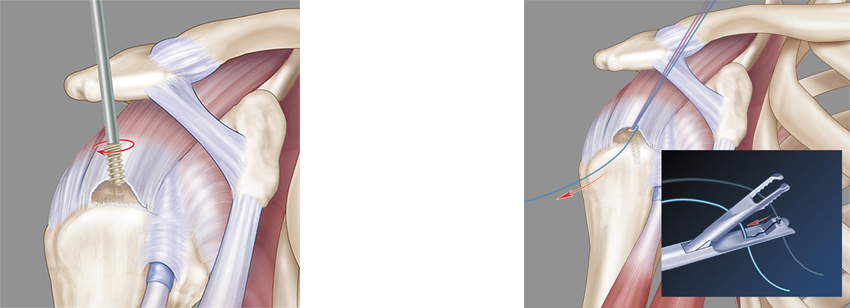
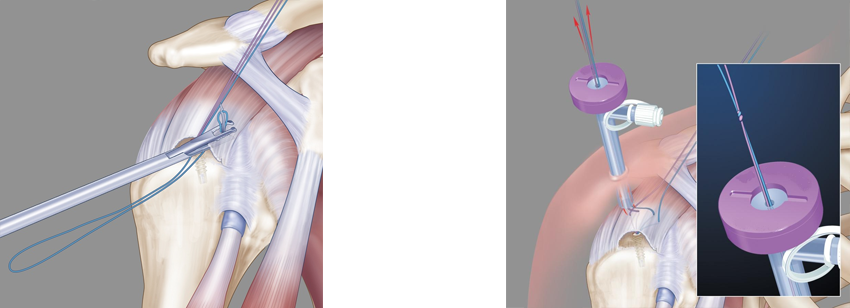
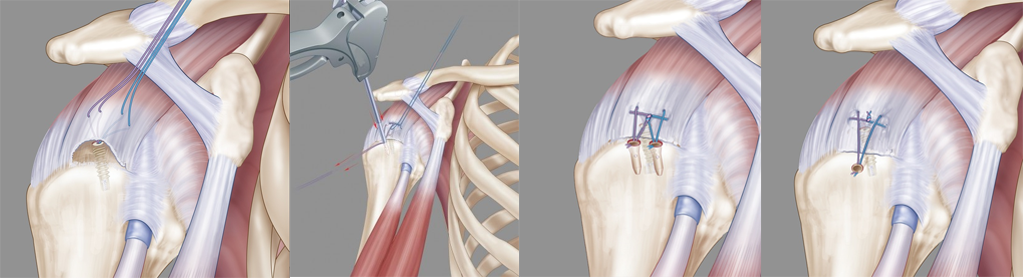
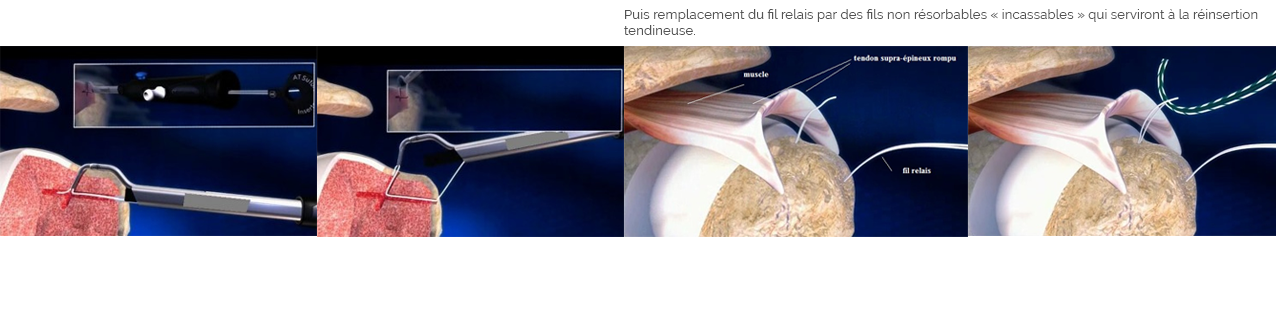
Tendon reinsertion with anchors
Proper tendon repair is the essential step in rotator cuff repair.
Whatever the technique used, it is a question of resetting the tendons on their area of bone insertion (tuberosity around the humeral head) that is called the foot print (impression left by the tendon on the bone)
You can see a re-insertion video on anchor by clicking: supra-thorny video
We will take as an example the repair of a U-shaped rupture of the supraspinous tendon as in the diagram below:
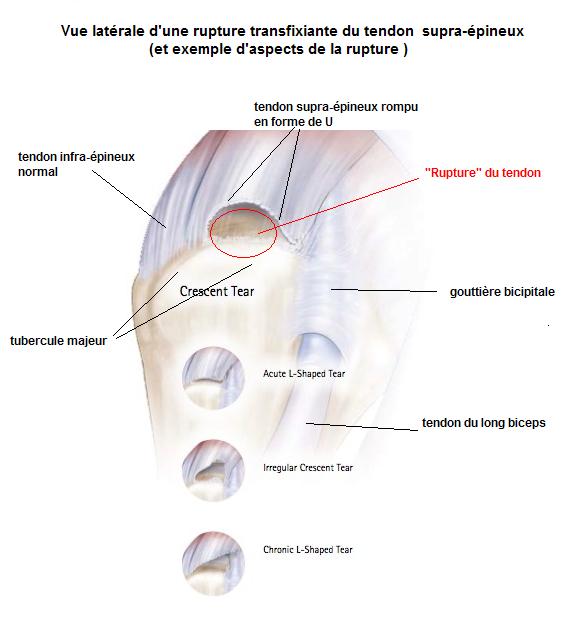
We can schematize in several steps:
1 / Avinence of bone tuberosities, place of insertion of the tendons (using an oscillating bur)
The aim is to cover as much as possible the normal foot-print (of the broken tendon) with tendinous tissue thus brought back.
The material and the threads are only there to force the tendons to heal on the bone, they do not have sufficient strength to sustainably maintain the tendon in place especially when using the limb.
The tendons are in principle firmly re-staged after 6 weeks.
NB: the drawings are kindly lent to us by one of our industrial partners marketing implants used.
Reinsertion cap without anchor
Proper tendon repair is the essential step in rotator cuff repair.
Whatever the technique used, it is a question of resetting the tendons on their area of bone insertion (tuberosity around the humeral head) that is called the foot print (impression left by the tendon on the bone)
We will take as an example the repair of a supraspinous tendon rupture:
We can schematize in several steps: